The Burdens of Chemical Toxicity for Children and Women
By Megan LeGresley
A couple of months ago, my mom forwarded me a link to a blog run by a young woman battling chronic Lyme disease and exposure to mold. She had severe chemical sensitivities, among many other symptoms. These sensitivities were so severe that she had to reset her entire autonomic nervous system by rewiring her limbic system–the part of the brain responsible emotional and behavioral responses–to turn off her body’s ongoing unconscious fight-or-flight response in order to be able to function in the elementary school at which she taught.
As I read her story, I was struck by the similarities to my own health conditions, not in the least the illness that results when I am exposed to chemicals in everyday products ranging from cleaning solutions to perfumes. I’ve scheduled time at the end of this quarter of college when I, too, can go through the same neurological reset process in search of relief from the often overwhelming sensations of dizziness, drowsiness, and devitalization stemming from unintentional and/or unavoidable chemical exposures.
Those with other underlying health conditions are only a fragment of the population that experiences sensitivity to chemicals. Often, we have Multiple Chemical Sensitivity (MCS) as an aspect of a broader disease paradigm, or can be made ill by chemical exposure in general. 80-90% of ingredients used to make the artificial fragrances developed in the past 50 years have been extracted from petroleum and/or tar. These ingredients are common indoor air pollutants. Their impact manifests as respiratory conditions, neurological impairment, and/or eye and skin irritation. In addition, over one-third of a sample of the U.S. population surveyed in 2016 reported problems including migraines and breathing trouble stemming from fragrances.
A 2009 meta-analysis from the University of Maryland reported that “the U.S. consumer is as uneducated about the dangers and health risks associated with constant exposure to the chemicals used in synthetic fragrance products as the average non-smoker was to the risks of secondhand smoke” (De Vader and Barker). The authors project that as knowledge moves from within the medical field to the lay population, as with the shift in smoking from normal to outlawed in many public locales, many people will again demand greater protections for the general well-being.
They also point out that unlike smoke, chemical exposure can function as an invisible phenomenon. The FDA does not require the labeling of specific chemicals found in fragrances, protecting such “secrets” under the generic term “fragrance.” One often cannot see the clouds of chemicals spewing into the air except under immediate extreme scenarios (picture the spraying of weed killers). Nevertheless, “a recent analysis of 6 top selling laundry products and air fresheners found nearly 100 volatile organic compounds [VOCs] were emitted from the products and five of the six products emitted one or more carcinogenic hazardous air pollutants which the Environmental Protection Agency considers to have no safe exposure level” (De Vader and Barker). And these are products specifically marketed as “fresh” and “clean!”
In 2006, a researcher at the Icahn School of Medicine at Mount Sinai in New York led a team identifying toxicants that negatively impact the health of children. They found that substances such as phthalates (endocrine disrupting compounds that maintain color and scent) linger from prenatal stages through childhood. Exposure can come from unexpected sources: for instance, breast milk feeds children the fats and sugars that their immune systems, cells, and nerves need to thrive – but it also exposes them to “paint thinners, dry-cleaning fluids, wood preservatives, toilet deodorizers, cosmetic additives, gasoline by-products, rocket fuel, termite poisons, [and] fungicides” that breastfeeding persons may have encountered throughout their lives. (Williams). Other sources of exposure can include swimming pools, sunscreens, pesticides, flame retardants in furniture, and drugs intended to prevent infection. In 2000, a committee of the U.S. National Academy of Sciences reported 25% of developmental defects may be due to the interaction of genetic factors and environmental factors, revealing the serious consequences of these everyday exposures.
Gender matters to our understandings of chemical exposure. As reported by The Economist in 2017, the sciences remain male-dominated, a phenomenon reflected in the authorship of research studies. At the same time, social pressure on women holds them responsible for the fetal environment.They are expected to protect fetuses as much as possible from the toxins we all carry in our bodies. A flyer distributed by Physicians for Social Responsibility specifically first questions “How are women exposed to environmental chemicals? Studies have shown that virtually all pregnant women in the U.S. have measurable levels of several toxins in their bodies that pose real threats to the development of the fetus. These dangerous chemicals include phthalates, bisphenol-A (BPA) and flame retardants. Their impacts can manifest in the short term as birth defects or later in life as problems with reproduction, obesity, diabetes, hormonal balance or even cancers.”
Due to socially prescribed disparities in the use of beauty products between men and women, women are exposed certain chemicals more than men. Yet should the onus to safeguard reproductive health just be placed on women? Men are mentioned only briefly towards the end of the aforementioned flyer: “Exposure to chemicals in everyday products like plastics can alter and weaken sperm, dramatically influencing the fertilized egg and development of the fetus.” All bodily fluids carry metals and chemicals. We must ask more inclusive, comprehensive, and efficacious questions.How are we all exposed to environmental chemicals? And how do we change this?
Simply sharing one’s experiences can be activist work. The more that people understand what others are feeling, the more that those with chemical sensitivities know they are not the only ones and that their bodies are not abnormal but in fact responding reasonably to threats to their well-being, the more progress can be made as we become aware, empowered, and committed to ensuring the safety of future generations. As new avenues of research – including oral history – open up to a more inclusive group of patients and activists, people who do not have access to scholarly journals can enrich and further inform conversations about the methods we can take to help one another breath, move, and live a little easier – and a little closer to nature. We are, after all, living on earth, not in Bath & Body Works.
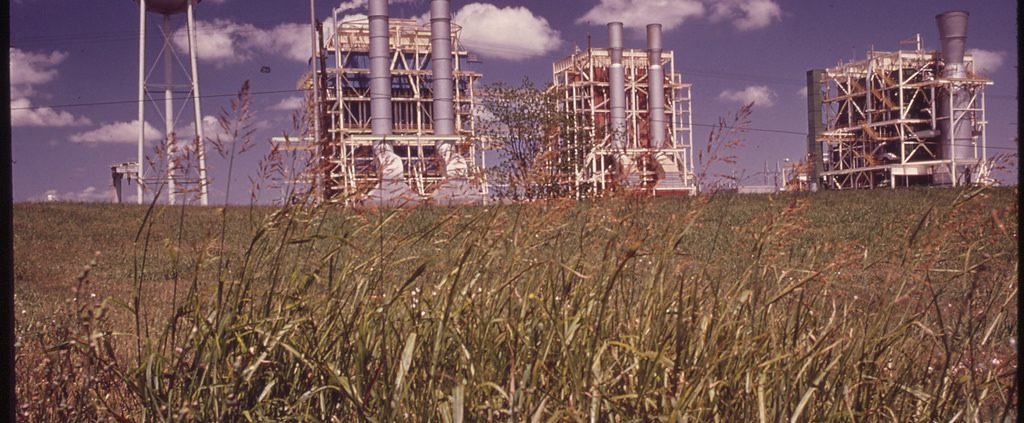
Image: Chemical Plants in Louisiana. U.S. National Archives.
Megan LeGresley is a member of the 2018-2019 Chemical Entanglements Undergraduate Research Group. She is a student in the departments of Economics and Political Science and UCLA.
Works Cited
Acosta, Annie. “30% increase in Autism rates brings urgency to chemical reform.” Safer Chemicals, Healthy Families, Safer Chemicals, Healthy Families, 9 Apr. 2014. Accessed 18 Nov. 2018.
“Asthma Facts and Figures.” Asthma and Allergy Foundation of America, Asthma and Allergy Foundation of America, Feb. 2018. Accessed 18 Nov. 2018.
Burrows, Sara. “Fragrance is the New Second-Hand Smoke.” Return to Now, Return to Now, 17 June 2018. Accessed 18 Nov. 2018.
De Vader, Christy L., and Paxson Barker. “Fragrance in the Workplace is the New Second-Hand Smoke.” American Society of Business and Behavioral Sciences, vol. 16, no. 1, Feb. Accessed 18 Nov. 2018.
“Dynamic Neural Retraining Systems: My 6-Month Update.” Resiliently Rachel, WordPress.com,14 Oct. 2018. Accessed 18 Nov. 2018.
EWG and the Campaign for Safe Cosmetics. “Not So Sexy: Hidden Chemicals in Perfume and Cologne.” EWG.org, Environmental Working Group, 12 May 2010. Accessed 18 Nov. 2018.
Gilton, Katie L. “The effect of chemical fragrances on child health and development.” University of Central Florida Showcase of Text, Archives, Research & Scholarship, 2011. Accessed 18 Nov. 2018.
Levitt, Janice. “Ingredients to avoid in personal care products and household cleaning products, and why this is so important.” Savor Wellness, Savor Wellness, 18 Mar. 2018. Accessed 18 Nov. 2018.
Lewandowski, TA, et al. “An evaluation of surrogate chemical exposure measures and autism prevalence in Texas.” Journal of Toxicology and Environmental Health, Part A, vol. 72, 24, 2009, pp. 1592-603. Accessed 18 Nov. 2018.
McCampbell, Ann. “What is Multiple Chemical Sensitivity?.” The Chemical Sensitivity Foundation, Chemical Sensitivity Foundation, 2018. Accessed 18 Nov. 2018.
Mercola, Dr. Joseph. “Is Your Perfume Poison?.” Mercola, Dr. Joseph Mercola, 27 Nov. 2013. Accessed 18 Nov. 2018.
Nasir, Adnan. “Nanotechnology in Vaccine Development: A Step Forward.” Journal of Investigative Discovery, vol. 129, no. 5, May 2009, pp. 1055-59. Accessed 18 Nov. 2018.
“Prenatal Exposure to Toxic Chemicals.” Physicians for Social Responsibility, Physicians for Social Responsibility, May 2018. Accessed 18 Nov. 2018.
“Science remains male-dominated.” The Economist, The Economist, 11 Mar. 2017. Accessed 18 Nov. 2018.
Sinrich, Jenn. “12 Toxic Ingredients Found in Your Beauty Products.” Reader’s Digest, Trusted Media Brands, Inc, 2018. Accessed 18 Nov. 2018.
St. Gil, Marc. Chemical Plants. 1973, The U.S. National Archives, College Park. Flickr Creative Commons, Accessed 18 Nov. 2018.
Steinemann, Anne. “Fragranced consumer products: exposures and effects from emissions.” Air Quality, Atmosphere & Health, vol. 9, no. 8, Dec. 2016, pp. 861-66. Accessed 18 Nov. 2018.
U.S. Food & Drug Administration. “Fragrances in Cosmetics.” FDA, U.S. Food & Drug Administration, 8 Aug. 2018. Accessed 18 Nov. 2018.
Williams, Florence. Breasts: A Natural and Unnatural History. New York City, W.W. Norton & Company, 2013, pp. 197-217.
Wolff, Mary S., et al. “Emerging Exposures of Developmental Toxicants.” Current Opinion in Pediatrics, vol. 29, no. 2, Apr. 2017, pp. 218-24. Accessed 18 Nov. 2018.
“Women, Health, and the Environment: Powerful voices for systematic change.” Women’s Voices for the Earth, 2018. Accessed 18 Nov. 2018.