Brain, Blood, and Self-Report: Gaining Insights into Stress-Related Cancer Outcomes in Female Breast Cancer Survivors
By Carrianne Leschak
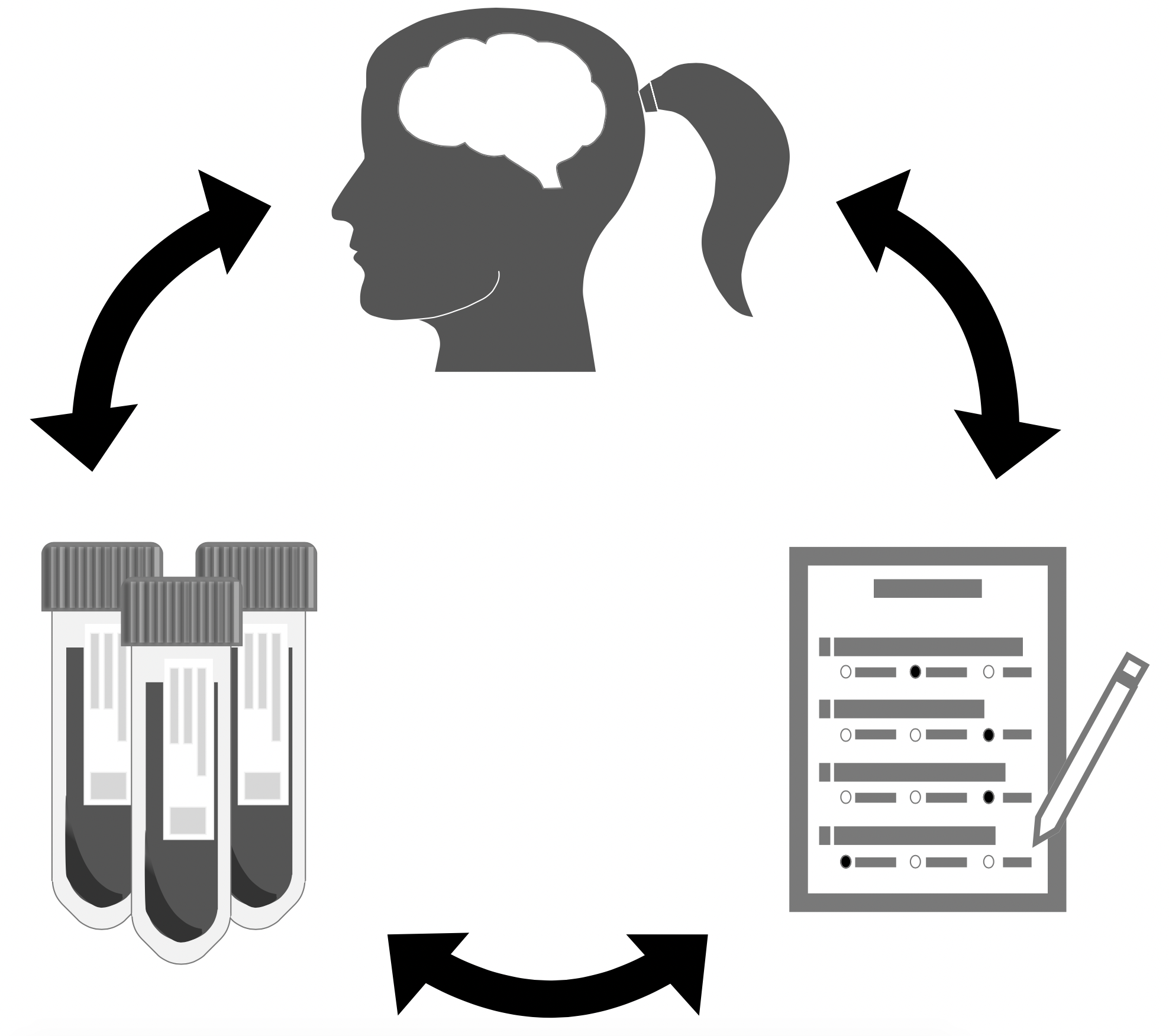
Rather than using a single methodology in research, integrating data from a combination of sources (e.g., biophysiological, behavioral, and self-report) can provide a more comprehensive understanding of how psychological experiences are related to health and well-being.
Beyond self-reports
If you ask someone to predict how they will feel in response to a certain event, or to predict what they will do in a certain situation, most people will give you an answer with some level of confidence. However, most will also be wrong. Psychology has shown us that we do not know ourselves as well as we think. For example, humans are not very good at affective forecasting—predicting how we will feel in the future—partly because of faulty assumptions we make by default.1 These assumptions are hidden to us in the present, so we do not realize our misguided predictions. This is just one example of the ways in which our self-knowledge is limited. In addition to misjudging the future, we also have difficulty remembering past experiences accurately,2 and sometimes do not understand the things we are doing as we are doing them.3 It is because of these cognitive and perceptual limitations in understanding ourselves (and often others) that the methodology we use to conduct psychological research becomes particularly important.
As a social psychologist, I am often trying to understand exactly why people do the things they do in different situations, how they will feel about it, and what other implications these psychological experiences can have, for example, on physical health. In doing this research, the simplicity of a self-report questionnaire measure can be ever so appealing. If you want to know how someone will react in a situation, just ask them. Self-report measures do have their place in research; if we want to know how people felt in the past, often all we have to rely on are retroactive self-reports. But, the utility of these measures can be augmented when we combine them with additional methods and measures to better understand what they are really telling us. This is why, in my own research, I rely on a multi-method approach that combines data from different sources and levels in order to gain a more complete understanding of social experiences and their impact. For example, to augment self-report data, I have collected various types of biophysiological data in order to better understand how stressful experiences may contribute to physical health markers that have been linked to breast cancer outcomes in women.
The current research
In this research, we recruited women from the greater Los Angeles area who were previously diagnosed with breast cancer but were not currently undergoing treatment. Examining breast cancer survivors is important because psychological experiences following treatment have been linked with future cancer recurrence,4 and post-treatment well-being in survivors.5 From past research, we knew that inflammation (the body’s natural response to try to fight off sickness or heal an injury) is linked with several cancer-related outcomes, including metastasis6 and overall survival.7 We also know that psychological stress initiates activation of the sympathetic nervous system (SNS), ultimately increasing circulating markers of inflammation.8 Thus, psychological stress might exacerbate tumor-relevant biological processes via inflammation. However, we wanted to better understand how the brain translates experiences of psychological stress into SNS activity and subsequent inflammation.
To do this, we focused on a circulating marker of inflammation called C-reactive protein (CRP). Although there are other markers of inflammation we can measure from plasma, CRP is an important prognostic marker for cancer-related outcomes in breast cancer survivors, such as cancer recurrence9 and fatigue.10 Within the brain, we specifically focused on the amygdala, a region that plays a role in SNS responding.11 Thus, we hypothesized that the amygdala might play a role in translating experiences of prolonged psychological stress into heightened levels of inflammation in breast cancer survivors. To test this, female breast cancer survivors completed a neuroimaging study in which they viewed socially threatening stimuli (fearful and angry faces), a task known to activate the amygdala.12 They also completed self-report measures of perceived stress over the previous month, and provided a blood sample that was analyzed for circulating levels of CRP in order to examine inflammation.
We found that women who reported being more stressed over the previous month tended to have higher levels of threat-related neural activity in the amygdala. In turn, women who had higher levels of threat-related amygdala reactivity tended to have higher levels of CRP, the inflammatory marker that has previously been linked to cancer outcomes. Interestingly, self-reports of prior stress were not directly linked with CRP in our study. In short, our data suggests that breast cancers survivors who experience greater levels of psychological stress may be further sensitized to social threats, as demonstrated by heightened amygdala activity. Furthermore, such heightened amygdala activity may coincide with greater levels of inflammation (e.g., CRP), which is likely to have implications for breast cancer recurrence and survivorship.
Our conscious awareness of our thoughts and feelings, which might be captured by self-report questionnaire measures, are only a fraction of our complete psychological experience. Understanding how complex interactions between our brain and our body influence, and are influenced by, our overt psychological experiences requires methodological approaches that can examine these systems simultaneously. For example, in order to better understand neuroimmune pathways through which psychological experiences might influence downstream cancer outcomes, we must implement multi-method approaches that combine self-reports with measures of functional brain activity and immunological activity within the body.
Carrianne Leschak is a PhD candidate in Social Psychology. She received her bachelor’s degree in Psychology, Sociology, and Criminology from the University of North Carolina Wilmington, and a master’s degree in Psychology from UCLA. Her research aims to understand the bidirectional relationship between social interactions and physical health. Leschak is the recipient of CSW’s 2019-2020 Elizabeth Blackwell, MD, Graduate Award.
- Timothy D. Wilson and Daniel T. Gilbert, “Affective Forecasting: Knowing What to Want,” Current Directions in Psychological Science 14, no. 3 (2005): 131-34.
- Yanchi Zhang, Zhe Pan, Kai Li, and Yongyu Guo, “Self-Serving Bias in Memories: Selectively Forgetting the Connection Between Negative Information and the Self,” Experimental Psychology 65, no. 4 (2018): 236-44.
- Timothy D. Wilson, Douglas J. Lisle, Jonathan W. Schooler, Sara D. Hodges, Kristen J. Klaaren, and Suzanne J. LaFleur, “Introspecting about Reasons Can Reduce Post-Choice Satisfaction,” Personality and Social PsychologyBulletin 19, no. 3 (1993): 331-39.
- Mogens Groenvold, Morten Aagaard Petersen, Ellen Idler, Jakob Bue Bjorner, Peter M. Fayers, and Henning T. Mouridsen, “Psychological Distress and Fatigue Predicted Recurrence and Survival in Primary Breast Cancer Patients,” Breast Cancer Research and Treatment 105 (2007): 209-19.
- Meghan H. McDonough, Catherine M. Sabiston, and Carsten Wrosch, “Predicting Changes in Posttraumatic Growth and Subjective Well-Being among Breast Cancer Survivors: The Role of Social Support and Stress,” Psycho-Oncology 23 (2014): 114-20.
- Raman Preet Kaur, Raja Paramjeet Singh Banipal, Rajesh Vashistha, Monisha Dhiman, and Anjana Munshi, “Association of Elevated Levels of C-Reactive Protein with Breast Cancer, Breast Cancer Subtypes, and Poor Outcome,” Current Problems in Cancer 43, no. 2 (April 2019): 123-29, https://doi.org/10.1016/j.currproblcancer.2018.05.003.
- Brandon L. Pierce, Rachel Ballard-Barbash, Leslie Bernstein, Richard N. Baumgartner, Marian L. Neuhouser, Mark H. Wener, Kathy B. Baumgartner et al., “Elevated Biomarkers of Inflammation Are Associated with Reduced Survival among Breast Cancer Patients,” Journal of Clinical Oncology 27, no. 21 (July 20, 2009): 3437-44, https://doi.org/10.1200/JCO.2008.18.9068.
- Andrew Steptoe, Mark Hamer, and Yoichi Chida, “The Effects of Acute Psychological Stress on Circulating Inflammatory Factors in Humans: A Review and Meta-Analysis,” Brain, Behavior, and Immunity 21, no. 7 (2007): 901-12, https://doi.org/10.1016/j.bbi.2007.03.011.
- Brandon L. Pierce, Rachel Ballard-Barbash, Leslie Bernstein, Richard N. Baumgartner, Marian L. Neuhouser, Mark H. Wener, Kathy B. Baumgartner et al., “Elevated Biomarkers of Inflammation Are Associated with Reduced Survival among Breast Cancer Patients,” Journal of Clinical Oncology 27, no. 21 (July 20, 2009): 3437-44, https://doi.org/10.1200/JCO.2008.18.9068.
- Ingrid J. Orre, Kristin V. Reinertsen, Pål Aukrust, Alv A. Dahl, Sophie D. Fosså, Thor Ueland, and Robert Murison, “Higher Levels of Fatigue Are Associated with Higher CRP Levels in Disease-Free Breast Cancer Survivors,” Journal of Psychosomatic Research 71, no. 3 (September 1, 2011): 136-41, https://doi.org/10.1016/J.JPSYCHORES.2011.04.003.
- M.R. Delgado, A. Olsson, and E.A. Phelps, “Extending Animal Models of Fear Conditioning to Humans,” Biological Psychology 73, no. 1 (July 2006): 39-48, https://doi.org/10.1016/j.biopsycho.2006.01.006.